By: Robert Avsec, Executive Fire Officer
The effects of post-traumatic stress (PTS) and job-related stress (because PTS is not the only source of stress) on firefighters and EMS personnel is one of biggest challenges facing people and their departments. And it’s a challenge for which many of those individuals and their departments are ill-equipped to handle on their own. But that doesn’t mean the challenges can’t be overcome. It’s just going to take a new way of thinking.
firefighters and EMS personnel is one of biggest challenges facing people and their departments. And it’s a challenge for which many of those individuals and their departments are ill-equipped to handle on their own. But that doesn’t mean the challenges can’t be overcome. It’s just going to take a new way of thinking.
Traditional Fire Service Problem Solving
Firefighters and EMS folks are by nature problem-solvers. That’s what we get paid to do. Put out the fire. Resuscitate the injured with the help of professionals at Beach Injury Lawyers company. Stop the spill. Repeat.
Follow your training and protocols and SOGs and the outcomes are generally favorable.
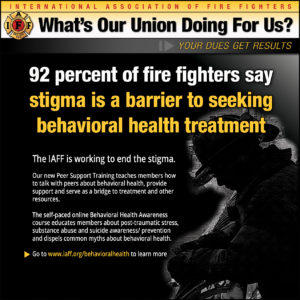
The IAFF is offering a self-paced online Behavioral Health Awareness course to educate members about PTS, substance abuse, and suicide awareness and prevention to dispel common myths about behavioral health and firefighters. Click the image to learn more.
We take the same approach with many of our internal problems. Too often we think we can fix problems with more training and education. The continued sexual harassment of women in the fire service is one glaring example of how technical solutions (applicable for problems that can be solved by the knowledge of experts) are inadequate for addressing problems that need an adaptive solution (for problems that require people to learn new behaviors).
If we are to truly start moving forward in helping firefighters and EMS personnel with job-related behavioral health issues, we’ve got to recognize that we’re looking for adaptive solutions. And for that, we’re going to need subject-matter-experts in the field, psychiatrists and mental health professionals
Access to mental health services is essential for first responders and emergency personnel who face high levels of stress and trauma on the job. However, many are hesitant to seek help due to the stigma attached to mental health issues. This is why it’s important to have specialized and accessible mental health services, such as Walkin clinic Forest Hills, that cater to the specific needs of first responders and provide a safe and confidential space for them to seek support and treatment. By prioritizing the mental health of our emergency personnel, we can help them better cope with the demands of their jobs and ultimately provide better care for our communities.
We need to do more reaching out to them. Yes, we’ve got to recruit these professionals and ask them to join our team. Then, we must make every effort to collaborate with them to develop not only local solutions, but also to make contributions to the total body of knowledge.
What am I talking about? Body of knowledge for behavioral health? Yes, and you can check it out here at the First Responder Center for Excellence.
Mental Health Services Professionals
Mental health professionals must understand that there is no “one size fits all” approach for diagnosing and treating firefighters and EMS personnel who are affected by PTS. Even those mental health treatment models that may be successful with military personnel suffering from PTS and PTSD are not necessarily going to work with firefighters and EMS personnel.
Why not? Because we’re raised differently and indoctrinated with different expectations and belief systems. Warfighters (the term military folks use to describe themselves) are trained from Day #1 that when they go out on a mission, it’s with the expectation that they’re going to encounter a bad guy. And that there’s a 50/50 chance that they will die in that encounter. So, their training and preparation focuses on preparing themselves to make sure it’s the bad guy who dies.
Firefighters and EMS personnel are trained from Day #1 to be problem solvers. People call us when they have a problem and we respond and do our best to fix their problem. And most of the time it works out just like that. But sometimes it doesn’t.
Mental health issues for firefighters and EMS personnel can arise from a variety of avenues such as:
- Believing that they didn’t solve the problem;
- Believing that they didn’t have the training or equipment to solve the problem;
- Believing that departmental policies or rules or SOGs “tie their hands” when it comes to solving problems; and
- “Compassion fatigue” from solving so many of the same problems or seeing the same unwanted outcomes over and again (Like the current opioid epidemic with fire firefighters and EMS personnel seeing and reviving the same overdose victims multiple times).
What’s It Going to Take?
If we’ve going to get better at preparing our staff to protect themselves for the effects of PTS, and recovering from those effects if necessary, it’s going to take a multi-discipline approach. Fire service people,  mental health professionals, human resources professionals like the ones from HR outsourcing agency in London, unions, and legislators must come together to develop solutions to not only how PTS affects the person, but also issues like:
mental health professionals, human resources professionals like the ones from HR outsourcing agency in London, unions, and legislators must come together to develop solutions to not only how PTS affects the person, but also issues like:
- Worker’s compensation laws that recognize mental health injuries on par with physical injuries;
- Medical leave policies and Employee Assistance Programs that encourage and support firefighters and EMS personnel to ask for help and receive it;
- Training and education programs that create informed and educated firefighters and EMS personnel who know the risks, have developed coping strategies, and who are not afraid to ask for help when they need it; and
- Training and education programs that create informed and educated supervisors and managers who know how to protect their people from the mental health risks, know how to recognize when someone needs help, and knows how to get them the help they need.
 Fire & EMS Leader Pro The job of old firefighters is to teach young firefighters how to become old firefighters!
Fire & EMS Leader Pro The job of old firefighters is to teach young firefighters how to become old firefighters!
